Mechanical thrombectomy is a recently implied method to open the blocked artery of the brain in stroke cases where thrombolysis (clot-busting drug) has failed or not suitable for it’s use to recanalise the blocked artery to reverse the stroke.
In cases of acute stroke which can be due to occlusion of main blood vessels of the brain, there is insufficient blood supply to the brain which cause permanent neurological damage if not opened in time. The thrombus(clot) can be removed using neurointervention techniques like suction thrombectomy or stent retrieval thrombectomy or it can be dissolved by intra-arterial administration of clot lytic drugs.
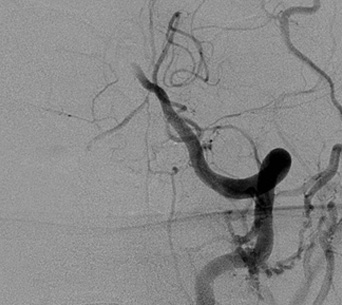
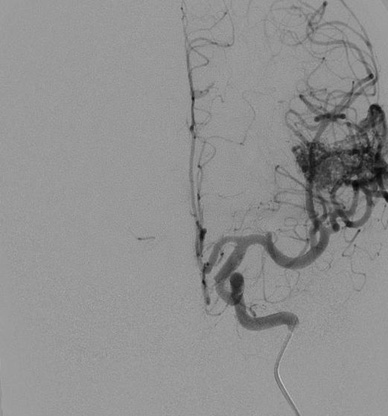
Left Vertebral artery angiogram showing complete occlusion of the Basilar artery
Left Vertebral artery angiogram showing complete restoration of flow of the Basilar artery after suction thrombectomy.

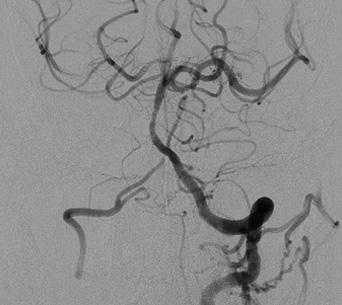
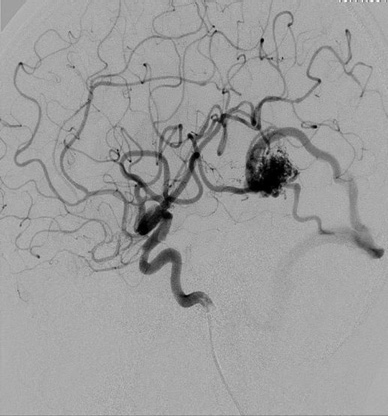
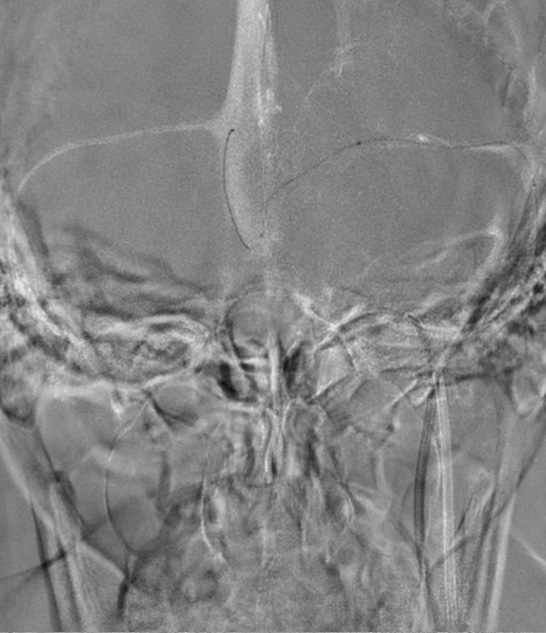
Right Carotid artery angiogram showing complete occlusion of the middle cerebral artery.

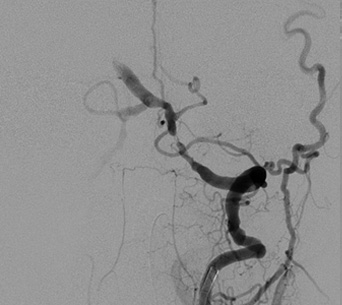
Right Carotid artery angiogram showing complete restoration of flow of the middle cerebral artery after combined suction and stent retriever thrombectomy.
Carotid atherosclerotic disease occurs when fatty deposits (plaques) clog the blood vessels that deliver blood to the brain and head (carotid arteries). Similarly the blockage can happen in vertebral artery as well. The blockage increases the risk of stroke, a medical emergency that occurs when the blood supply to the brain is interrupted or seriously reduced. The first sign that one have for this condition may be a stroke or transient ischemic attack (TIA). Mild and moderate stenosis (unto 70%) is treated with medical therapy but if stenosis increases to more than 70% in symptomatic cases and more than 80% in asymptomatic patients then only secondary prevention is recommended by surgery or intervention.
There are two options of dealing this blockage in the brain arteries: 1- Surgery: carotid Endarterectomy an old, conventional method and 2- Intervention: Carotid Stenting and angioplasty.
Both procedures are effective and safe in experienced hands, but carotid stenting is minimally invasive and short hospital stay (2days) procedure and generally preferred now a days. However, if blockage is highly calcific then we prefer surgery over intervention

Left Carotid artery angiogram showing critical stenosis (>95%) of the internal carotid artery - Before Stenting

Left Carotid artery angiogram - After Stenting and angioplasty
Left vertebral artery angiogram showing critical stenosis of left V4 segment of vertebral artery

Intra cranial angioplasty and stenting done with near complete recanalization of left vertebral artery.
An aneurysm is a weakened area in the wall of an artery making it prone for rupture. If an aneurysm ruptures, it can cause life-threatening bleeding and brain damage. The goal of aneurysm tretment is to isolate an aneurysm from the normal circulation without blocking off any small arteries nearby or narrowing the main vessel by accessing the aneurysm from within the bloodstream either by surgical clipping or by endovascular Coiling.
Endovascular Coiling is minimally invasive and does not require opening of the skull to reach the aneurysm. The aneurysm is reached through a blood vessel in the groin endovascularly. A flexible guiding catheter is advanced from the femoral artery to one of four arteries in the neck that lead to the brain and visualises the blood vessels of the brain by contrast injection. This provides us with a roadmap of the arteries. Subsequently a very tiny micro catheter is navigated through the guiding catheter into the aneurysm sac under Road-Map (A fluoroscopic shadow of contrast superimposed over the live fluoroscopy). Then through the micro catheter delicate platinum coils of different sizes and shape selected according to the morphology and diameter of aneurysm sac, are implanted one after the other till the aneurysm sac is fully filled with the coils and on contrast angiography no contrast is visible to enter the sac. The aneurysm is thus excluded from the circulation, effectively removing the risk of aneurysm rupture.
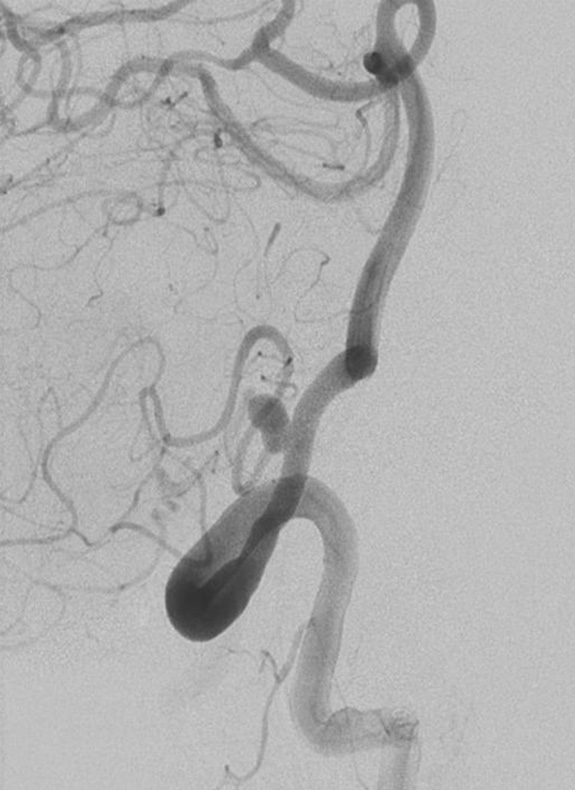
Right vertebral angiogram showing PICA (Posterior Inferior Cerebellar Artery) aneurysm.
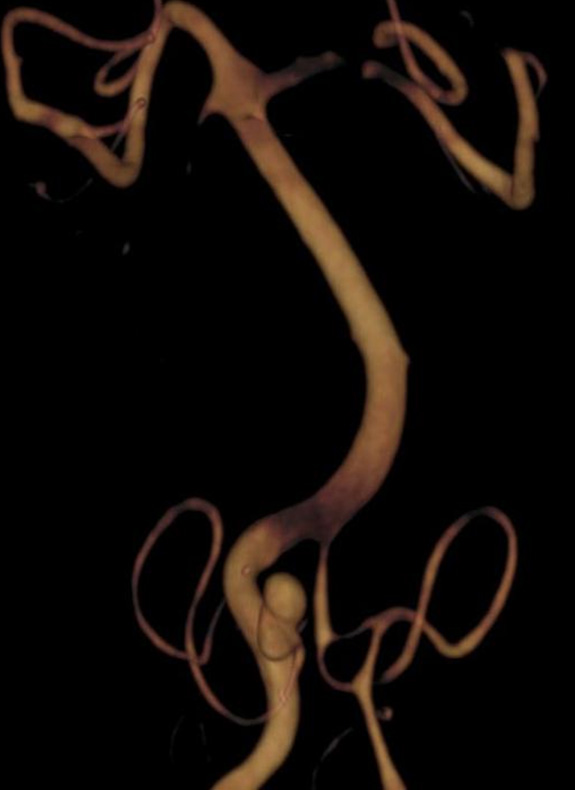
3D Rotational angiogram showing right PICA (Posterior Inferior Cerebellar Artery) aneurysm at the origin.

Post endovascular coiling of PICA (Posterior Inferior Cerebellar Artery) aneurysm
Flow diversion is a technique in which a device - Flow diverter stent (a soft, flexible mesh tube) is placed into the blood vessel with the help of a catheter introduced through a groin vessel, where an aneurysm has formed.
This process immediately diverts the flow of blood away from the aneurysm itself thus gradually causing remodelling of the diseased vessel.
This helps to treat complex aneurysms which are difficult to treat previously by simple coiling or conventional neurosurgery.
Arteriovenous malformations (AVMs) of the brain refer to abnormal connections between arteries and veins bypassing the normal capillary network to the brain parenchyma.
Brain AVMs commonly present with seizures or epilepsy which generally gets controlled with anti-epileptic drugs. However is some cases it may cause bleeding into or around the brain, most commonly in young adults which can cause headache or neurological deficits. Left untreated, there is a risk that they may bleed again causing severe neurologic damage and even death.
Conventionally AVMs were treated with microsurgical excision. Surgical excision of these clusters of vessels is a bloody surgery and often incomplete due to obscuration of surgical filed by bleeding when excision is done with knife /scisors. Moreover, some of the deep located AVMs are difficult to excise without any neurological morbidity. There was always a need of alternative treatment strategy in these complex and large vascular lesions. In recent past two methods came into practice which are minimally invasive. 1- Stereotactic Radiosurgery (SRS9 or Gamma Knife/Cyberknife Radiosurgery. In this under a highly sophisticated equipment Gamma rays radiation is given to the AVM nidus in a precisely defined way through multiple directions to avoid brain injury. This technique if effective in small AVM in about 80% cases over 2 years duration after SRS.
2- Endovascular AVM Embolisation: Embolization is a method of plugging the nidus of the AVM with glue or other liquid embolic agents like Onyx/Squid etc. under fluoroscopic guidance by a small tube called a flow guided micro-catheter. This method may require multiple microcatheterization to achieve complete results. Sometimes complete AVM embolisation may not be achieved safely in one session and embolisation may be repeated for the second time in some cases. THis require enormous expertise and deep knowledge of the microvascular anatomy and is generally safe to perform in high volume centres by experienced neurointerventionist.
DSA AP view of left ICA injection showing sulcal AVM with feeders from the left MCA
DSA Lateral view showing temporal branch feeding the AVM and large veins seen draining the nidus of the AVM in to the transverse sinus
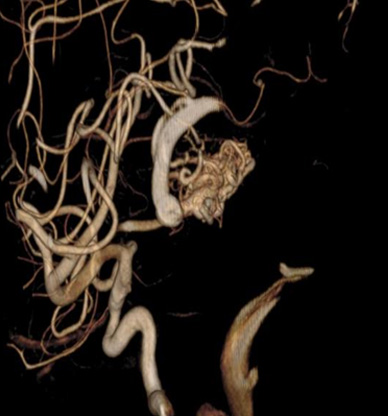
Reconstructed 3D Rotational angiogram showing the cerebral AVM
Spinal arteriovenous malformation (AVM) is a tangle of blood vessels on, in or near the spinal cord. Oxygen-rich blood usually enters the spinal cord through arteries, which branch into smaller blood vessels (capillaries). The spinal cord uses the oxygen from the blood in the capillaries. The blood then passes into veins that drain blood away from the spinal cord to the heart and lungs.
In a spinal AVM, the blood passes directly from the arteries to the veins and goes around the capillaries.If untreated, it can cause permanent weakness of limbs, loss of bladder & bowel function. Spinal arteriovenous malformations can be difficult to diagnose because the symptoms are similar to those of other spinal conditions, such as spinal dural arteriovenous fistula, spinal stenosis, multiple sclerosis or a spinal cord tumor.
In an angiography, a catheter is inserted into an artery in the groin and guided to the spinal cord. Dye is injected into blood vessels in the spinal cord to visualise under X-ray imaging. In the same sitting, these abnormal communications can be blocked by glue injection, thus restoring the normal blood supply of spinal cord.


Many brain tumors bleed heavily during surgery. This can make the neurosurgery very difficult. This difficulty can be eased by embolization (blocking) of the blood vessels feeding these tumors before surgery begins.
A cerebral tumor embolization is a procedure in which a catheter is placed into the patient's groin and carefully navigated into the blood vessels supplying the tumor under X-ray guidance. An angiogram is obtained by injecting X-ray dye into the blood vessel to examine the blood supply of the tumor and verify that it is safe to eliminate that vessel. Material is then injected through the catheter to block the blood vessel under X-ray guidance. Also chemotherapeutic drugs can be injected into the blood vessel supplying the tumor as an adjuvant or neoadjuvant therapy.


Image: Cerebral angiogram showing Chemoembolisation of convexity meningioma Pre (A) and Post (B)
Chronic subdural hematoma (cSDH) is a debilitating condition with a high rate of recurrence after surgical evacuation.The new procedure, MMA embolization, involves guiding a catheter that is inserted into a blood vessel to the area of the brain that is supplying blood to the subdural hematoma. Particles or a special type of glue will be released to stop the bleeding that is causing the subdural hematoma, thus preventing recurrence.
Cushing disease results from excessive cortisol production due to elevated ACTH levels produced by a pituitary tumor. In contrast, Cushing syndrome includes all conditions of hypercortisolism due to either ACTH-dependent causes (eg, Cushing disease or ectopic ACTH secretion by a nonpituitary tumor) or ACTH-independent causes (eg, excessive autonomous secretion of cortisol from a hyperfunctioning adrenocortical tumor). Inferior petrosal sinus sampling (IPSS) is an invasive procedure in which adrenocorticotropic hormone (ACTH) levels are sampled from the veins that drain the pituitary gland; these levels are then compared with the ACTH levels in the peripheral blood to determine whether a pituitary tumor (as opposed to an ectopic source of ACTH) is responsible for ACTH-dependent Cushing syndrome. IPSS can reliably establish on which side of the pituitary gland the tumor is located.
Cerebral DSA can be useful in assessing venous sinus stenosis which has implication in the etiopathogenesis of Idiopathic Intracranial Hypertension (IIH). Subsequent intracranial venous sinus manometry to assess the venous pressure gradient is important to guide the therapy in the form of Venous angioplasty and stenting, if needed.
DSA Showing Venous phase roadmap for navigation of the micro catheter into the intra cranial sinuses for Sinus Manometry in a case of drug refractory Idiopathic Intracranial Hypertension

Micro catheter selective injection in the Right Transverse Sinus